Liver cirrhosis is a condition where the liver gets scarred and doesn’t work as well as it should. This scarring happens slowly over time, often due to long-term damage from alcohol, infections, or other health problems. The liver is a crucial organ that helps clean toxins from the blood, digest food, and store important nutrients. When cirrhosis occurs, these functions are disrupted, which can lead to serious health issues.
In this guide, we’ll break down what liver cirrhosis is, how it’s diagnosed, the stages of the disease, and how it can be treated.
What Causes Liver Cirrhosis?
There are several reasons why someone may develop liver cirrhosis. Here are the most common causes:
- Chronic alcohol use: Drinking too much alcohol over a long period can damage the liver.
- Hepatitis infections (B and C): These viral infections cause long-term liver inflammation, which can lead to scarring.
- Non-alcoholic fatty liver disease (NAFLD): This happens when fat builds up in the liver, leading to damage.
- Autoimmune liver disease: In some cases, the body’s immune system mistakenly attacks healthy liver cells.
- Genetic conditions: Some people inherit conditions like Wilson’s disease or hemochromatosis, where harmful substances collect in the liver.
- Problems with bile ducts: If bile can’t flow properly through the liver, it can cause damage.
Symptoms of Liver Cirrhosis
Liver cirrhosis often doesn’t cause noticeable symptoms until significant damage has been done. However, as the disease worsens, symptoms may start to appear. These include:
- Feeling tired and weak
- Easy bruising or bleeding
- Yellowing of the skin and eyes (jaundice)
- Swelling in the abdomen or legs
- Nausea or vomiting
- Loss of appetite
- Itchy skin
- Dark-colored urine
- Difficulty thinking clearly (due to toxins building up in the brain)
If you notice any of these symptoms, it’s important to see a gastroenterologist in Surat or another liver specialist, especially if you have risk factors like heavy alcohol use or hepatitis.
How Is Liver Cirrhosis Diagnosed?
Diagnosing liver cirrhosis involves a few different steps:
- Blood tests: These check liver function and can look for signs of liver damage or infections like hepatitis.
- Imaging tests: An ultrasound, CT scan, or MRI can give a clear picture of the liver’s condition.
- Liver biopsy: In some cases, a small piece of liver tissue may be taken to confirm the diagnosis.
- Endoscopy: A flexible tube with a camera can be used to check for swollen veins (varices) in the esophagus, which often occurs in advanced cirrhosis.
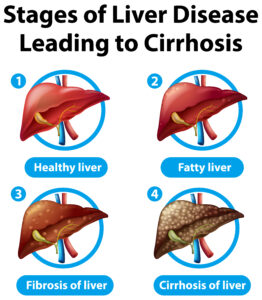
Stages of Liver Cirrhosis
Liver cirrhosis goes through different stages, from mild to severe:
- Compensated cirrhosis: At this stage, the liver is scarred but can still perform most of its functions. People in this stage may not have many symptoms and can often continue their daily activities.
- Decompensated cirrhosis: At this point, the liver can’t keep up with its tasks, and symptoms like jaundice, fluid buildup in the abdomen, and confusion become more noticeable.
- End-stage liver disease: This is the most serious stage of cirrhosis, where the liver completely fails. At this point, a liver transplant may be necessary.
Complications of Liver Cirrhosis
Without proper care, liver cirrhosis can lead to serious complications, such as:
- Portal hypertension: This happens when the blood pressure in the veins going to the liver becomes too high.
- Ascites: Fluid can build up in the abdomen, causing discomfort and increasing the risk of infections.
- Hepatic encephalopathy: The liver can no longer remove toxins from the blood, leading to confusion or even coma.
- Variceal bleeding: Swollen veins in the esophagus can rupture, leading to life-threatening bleeding.
- Liver cancer: People with cirrhosis are at a higher risk of developing liver cancer, especially if they also have hepatitis B or C.
Treatment Options for Liver Cirrhosis
While liver cirrhosis cannot be fully cured, early treatment can slow its progression and improve quality of life. Treatment focuses on managing the cause of the disease, controlling symptoms, and preventing complications.
- Lifestyle Changes:
- Avoid alcohol: If alcohol is the cause of cirrhosis, it’s critical to stop drinking completely.
- Healthy eating: A balanced diet low in salt can help reduce swelling and prevent malnutrition.
- Exercise: Regular physical activity can help prevent muscle loss, which is common in cirrhosis.
- Treating underlying conditions: Taking medications for hepatitis or managing obesity can prevent further damage to the liver.
- Medications:
- Antiviral drugs can be prescribed to treat hepatitis infections.
- Diuretics help reduce fluid buildup in the abdomen.
- Beta-blockers may be used to lower the risk of variceal bleeding in patients with portal hypertension.
- Procedures and Surgery:
- Endoscopic treatment: This can be used to stop bleeding from enlarged veins in the esophagus or stomach.
- Liver transplant: For those with end-stage liver disease, a transplant may be the only option for survival.
- Regular Monitoring: People with cirrhosis need regular check-ups to monitor liver function, spot complications early, and receive timely treatment.
Conclusion
Liver cirrhosis is a serious condition, but with the right care and lifestyle changes, its progression can be slowed, and complications can be managed. Early diagnosis and regular monitoring are essential for maintaining quality of life. If you have symptoms of cirrhosis or are at risk due to alcohol use, hepatitis, or other factors, it’s crucial to consult a gastroenterologist in Surat or your local liver specialist for advice and treatment.
Taking action early can make a significant difference, allowing you to manage the condition and live a healthier life.
